The opioid crisis has emerged as a significant public health emergency, deeply impacting various demographics including military veterans. Those who have served in the armed forces may be particularly vulnerable to opioid dependency and substance abuse due to a myriad of factors related to military service, including physical injuries, psychological trauma, and a general struggle to reintegrate into civilian life.
Veterans are often prescribed opioids for pain management following service-related injuries. However, the ease of access to these opioid prescriptions coupled with the high prevalence of chronic pain conditions can lead to increased rates of addiction. The physical and mental toll of military experience tends to create a perfect storm for opioid abuse.
The Challenges of Transitioning Back to Civilian Life
Many veterans do not receive adequate support when transitioning to civilian healthcare systems, leaving them at a heightened risk of addiction and related health complications. In addition to the challenges of accessing appropriate healthcare, veterans often grapple with feelings of isolation and stigma surrounding mental health issues. Many may feel reluctant to seek help for fear of being perceived as weak or unfit for civilian life. This stigma can prevent them from accessing vital resources, such as counseling or support groups, which could help them cope with both their physical and emotional pain.
The opioid crisis has far-reaching implications for families and communities connected to veterans. The impact of addiction can strain relationships, leading to familial discord and emotional distress for loved ones. Children of veterans struggling with addiction may experience instability and trauma, perpetuating cycles of hardship that can affect future generations. This is why family therapy can be essential for healing from addiction and overdose prevention.
The Opioid Addiction Epidemic in Utah
Utah has been one of the states hit hardest by the opioid epidemic. A large population of veterans, combined with rural areas that experience higher rates of isolation, can contribute to the rising rates of addiction. There’s no universal profile of someone susceptible to opioid overdose. But risk factors include pain conditions that require prescription drugs, which can apply to many veterans.
The stigma surrounding addiction often prevents individuals from seeking help. It can be particularly pronounced in rural communities, where tight-knit social structures may discourage open discussions about mental health and substance use. Telehealth services have emerged as an emerging solution to bridge these gaps, although access and efficacy can still be uneven across the state. The intent is to provide support as early as possible so that an opioid overdose is prevented before the addiction can develop. It may also speak to any desire to self-medicate via opioids, connecting addicted individuals with pain or mental health solutions before there is the risk of addiction or overdose.
Utah’s unique cultural landscape, heavily influenced by religious communities, plays a significant role in shaping attitudes toward substance use and recovery. Some programs that integrate faith-based approaches with evidence-based treatment have emerged, aiming to provide holistic support for those struggling with addiction. These initiatives address the physical aspects of addiction but can also emphasize spiritual and emotional healing.
The Opioid Epidemic’s Impact on Veterans

The opioid epidemic has had a devastating impact on veterans, with a disproportionate number of service members struggling with opioid use disorder. According to the Veterans Affairs (VA) department, the rate of opioid-related overdose deaths among veterans increased by 53% from 2010 to 2019.
The opioid crisis has also had a significant impact on the mental health of veterans. Many veterans struggle with mental health problems, such as post-traumatic stress disorder (PTSD), depression, and anxiety, which can increase the risk of opioid addiction. The stigma surrounding mental health disorders and substance use disorders can prevent veterans from seeking help, exacerbating the problem.
Who is Most Affected by the Opioid Crisis?
The opioid crisis affects a wide range of individuals, but certain groups face particular risks. Among these groups, some veterans stand out due to unique challenges associated with military service:
- Combat Veterans: Those who have experienced combat are often diagnosed with PTSD, which can drive them to seek relief through opioids.
- Older Veterans: Aging veterans may deal with chronic pain conditions, leading to higher rates of opioid prescriptions.
- Veterans in Rural Areas: Those living in less accessible areas might rely on opioids due to limited healthcare options.
Many people with conditions such as anxiety, depression, or bipolar disorder may turn to opioids as a form of self-medication, seeking temporary relief from their symptoms. This can lead to a dangerous cycle where the initial relief from pain or emotional distress ultimately results in increased dependency and more severe mental health challenges. Addressing the opioid crisis thus requires a comprehensive understanding of mental health and addiction, emphasizing the need for dual diagnosis treatment approaches that consider both physical and psychological health.
Why Are Veterans Prescribed Opioids?
Veterans are prescribed opioids for various reasons, primarily due to the injuries sustained during service. Many veterans experience ailments such as chronic pain, which can stem from physical conditions or combat-related injuries. Opioids are often considered effective for pain relief, but their potency comes with risks.
Broader societal trends and the ongoing opioid crisis influence the landscape of opioid prescriptions for veterans. As awareness grows about the potential for addiction and the dangers associated with long-term opioid use, there is a push for more holistic and multidisciplinary approaches to pain management. Initiatives such as physical therapy, acupuncture, and cognitive behavioral therapy (CBT) are gaining traction as viable alternatives, yet many veterans may still find themselves in a system that defaults to medication as a quick fix.
Chronic Pain and Opioid Addiction in Veterans
Chronic pain is a common issue among veterans, with many service members experiencing chronic pain as a result of injuries sustained during military service. While prescription opioids may be prescribed to manage chronic pain, they can also contribute to the development of opioid addiction. In fact, chronic pain patients are at a higher risk of developing opioid use disorder, particularly if they have a history of mental health problems or substance abuse.
The relationship between chronic pain and opioid addiction is complex, and addressing both issues simultaneously is crucial. The VA has implemented alternative pain management strategies, such as acupuncture, physical therapy, and cognitive-behavioral therapy, to help veterans manage chronic pain without relying on opioids. A holistic approach is essential to ensure that veterans receive the care and support they need to lead healthier, more fulfilling lives.
Opioid Addiction Support for Veterans
Recognizing the unique challenges faced by veterans struggling with opioid addiction, various support services are available. The Department of Veterans Affairs offers multiple programs designed to address both the physical and psychological aspects of addiction:
- VA Treatment Facilities: These specialized programs focus on recovery and often integrate therapy specific to veterans’ experiences.
- Medication-Assisted Treatment (MAT): MAT can provide veterans with medications to manage withdrawal symptoms, combined with counseling services.
- Peer Support Groups: Engaging with fellow veterans who have undergone similar experiences can foster a sense of community and belonging.
It is crucial for veterans to seek assistance and utilize the programs available to them. Support services can significantly impact recovery and help veterans navigate the path toward healthier choices.
In addition to these structured programs, many veterans find solace in holistic approaches that complement traditional treatment. Mindfulness practices, such as yoga and meditation, have gained traction as effective tools for managing stress and anxiety, which often accompany addiction. These practices not only promote mental well-being but also help veterans reconnect with their bodies, enhancing their overall recovery journey. Furthermore, outdoor therapy programs, which leverage nature as a healing environment, have shown promising results in reducing symptoms of PTSD and addiction, allowing veterans to bond with peers while engaging in physical activity.
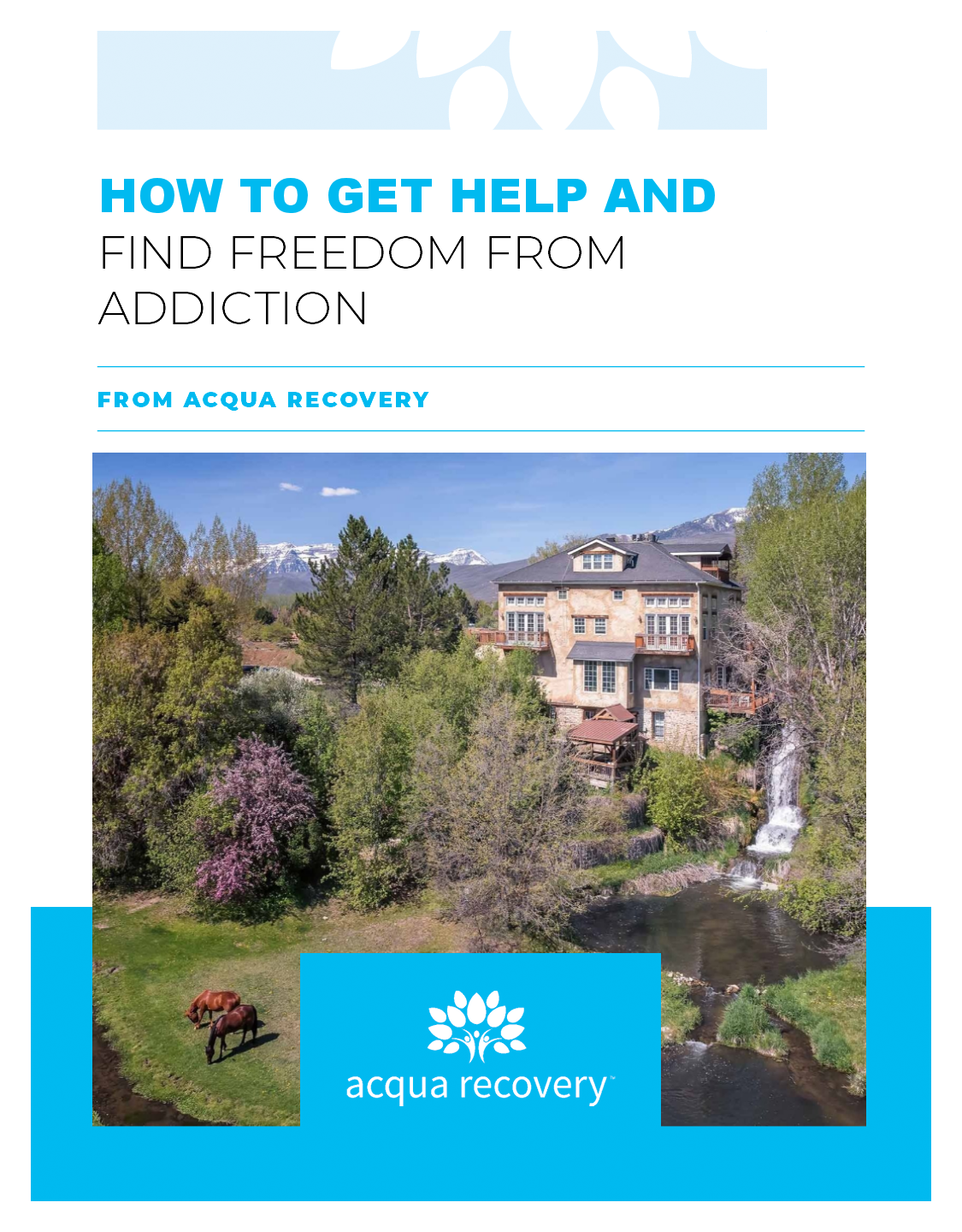
Addiction Rehab in Utah for Veterans at Acqua Recovery

As the opioid crisis continues to evolve, it is imperative for veterans and their advocates to remain vigilant and informed about the resources available to them. Addressing the crisis directly will require concerted efforts at all levels of society, fostering greater awareness and providing meaningful support to those who have served our country.
At Acqua Recovery, we’re committed to supporting people working toward a healthy recovery. Veterans deserve focused care that caters to their needs. Dual diagnosis treatment helps provide comprehensive, holistic care that addresses the special issues they face. Contact us today to learn more.