Addiction is a complex condition that affects millions of individuals worldwide. It impacts a person’s physical health, mental well-being, and social relationships. Among the various substances that can lead to dependency, some drugs are notably more challenging to quit than others. This could be due to their chemical composition or the intensity of cravings they provoke.
Understanding which drugs are hardest to quit is crucial in addressing addiction; it can inform treatment approaches and support strategies. This emphasizes the importance of tailor-fit treatment for those struggling to overcome their substance use. For this reason, examining the factors that contribute to their addictive properties is imperative. It’s also important to grasp the significant role they play in the much larger realm of addiction treatment.
A Bird’s Eye View on the Hardest Drugs to Quit
Drugs are difficult to quit once you’re hooked. This can be due to psychological factors or physical dependency. Some of the hardest drugs to quit include the following:
- Heroin
- Cocaine
- Methamphetamine
- Opioids
- Benzos
Heroin addiction is a chronic condition characterized by an overwhelming desire to use heroin. Heroin is a powerful opiate derived from morphine. Those struggling with heroin addiction experience intense cravings; they may even continue using the drug despite facing significant personal, health, and legal consequences.
Heroin alters the brain’s natural reward system, leading to changes in mood, behavior, and overall functioning. This addiction can cause both physical dependence and psychological reliance, making it incredibly challenging to overcome. Treatment typically involves a combination of medical intervention, counseling, and support services. Treatment for heroin addiction exists to address the multifaceted nature of addiction and assist individuals in reclaiming their lives.
Why is Heroin a Difficult Drug to Quit?
Heroin is difficult to quit due to its powerful addictive properties and the impact it has on the brain. When used, heroin rapidly crosses the blood-brain barrier, leading to intense feelings of euphoria and well-being. This immediate gratification reinforces the behavior, making users crave the drug even more. Additionally, the withdrawal symptoms that occur when attempting to quit can be extremely severe. These include intense cravings, nausea, sweating, and anxiety, which, oftentimes, can deter individuals from seeking help.
The psychological dependency that develops alongside physical addiction complicates recovery; users often resort to heroin as a coping mechanism for underlying issues such as trauma or mental health disorders. The combination of physical dependence, psychological factors, and withdrawal challenges imposes a barrier on those looking to recover from heroin addiction.
The most common types of medication to treat ADHD are stimulants such as Methylphenidate (Ritalin, Concerta) and Amphetamines (Adderall, Vyvanse). These medications work by increasing the levels of certain neurotransmitters in the brain, notably dopamine and norepinephrine, which play key roles in attention and behavior regulation. Stimulant medications have a high success rate, improving symptoms in about 70-80% of patients.
Similar to all medications, stimulants can present side effects and require a healthcare provider to monitor how an individual is reacting to the medication. As with all prescription medications, individuals must disclose other medications they are currently taking to avoid potential interactions. Some medications for common adult health problems can interact with stimulants, such as:
- High blood pressure medication
- Diabetes medication
- Depression medication
- Anxiety medication
Non-stimulant medications are also available for adults struggling with ADHD. Some options include Atomoxetine (Strattera), Guanfacine (Intuniv), and Clonidine (Kapvay). These medications work by targeting norepinephrine pathways more directly or affecting other neurotransmitter systems. Non-stimulants can be effective for patients who do not respond well to stimulants or have coexisting conditions like anxiety.
Cocaine addiction is a serious substance use disorder characterized by an overwhelming desire to consume cocaine. Cocaine is a powerful stimulant derived from the coca plant; it affects the brain’s reward system by increasing levels of dopamine, a neurotransmitter associated with pleasure and motivation.
Over time, individuals may develop tolerance, requiring higher doses to achieve the same euphoric effects, leading to a cycle of dependency. The addiction can result in various physical and psychological issues, including cardiovascular problems, anxiety, and mood disorders. Treatment often involves a combination of behavioral therapies, support groups, and medically assisted detox.
Why is Cocaine a Difficult Drug to Quit?
Cocaine is notoriously challenging to quit due to its powerful impact on the brain’s reward system. When consumed, it floods the brain with dopamine, a neurotransmitter associated with pleasure and reward, leading to intense feelings of euphoria. This dramatic increase in dopamine reinforces the behavior, making users crave the drug to replicate the experience.
Methamphetamine addiction is characterized by a compulsive need to use methamphetamine. Methamphetamine, also known as meth, is a powerful and highly addictive central nervous system stimulant. This addiction can lead to significant physical and psychological health issues. These health issues could include severe dental problems, weight loss, increased heart rate, anxiety, and paranoia. Those struggling with meth addiction may experience intense cravings and withdrawal symptoms. This makes it difficult to stop using the drug without professional help.
Why is Meth a Difficult Drug to Quit?
Meth poses significant challenges for those who want to quit due to its highly addictive nature and effects on the mind. The drug increases the release of dopamine significantly more than many other substances. This intense release creates powerful cravings, making quitting difficult. Additionally, prolonged use leads to changes in brain structure and function, impacting emotions and decision-making processes. This can result in withdrawal symptoms that are both physically and psychologically distressing.
Opioid addiction is when a compulsive pattern of opioid use develops despite harmful consequences. Opioids are a class of drugs that include both prescription pain relievers, such as oxycodone and morphine, and substances like heroin. Individuals struggling with opioid addiction may experience a range of symptoms, including increased tolerance to the drug, withdrawal symptoms when not using, and an overwhelming desire or craving for opioids. This condition can significantly impair one’s daily functioning and relationships.
Why are Opioids Difficult Drugs to Quit?
Opioids are notoriously difficult to quit due to their profound effects on the brain’s reward system. When used, they release large amounts of dopamine, creating intense feelings of pleasure and euphoria. Over time, the brain adapts to these substances, leading to physical dependence and tolerance, which means that higher doses are required to achieve the same effects.Withdrawal symptoms are also just as pervasive with this substance as they are with others. The intense discomfort associated with withdrawal contributes significantly to the difficulty many individuals face when attempting to quit opioids.
Benzodiazepines (benzos) are a class of medications often prescribed for anxiety, insomnia, and other related issues. While these drugs can be effective for short-term relief, prolonged use can lead to physical dependence and psychological cravings. Individuals may find themselves needing increasingly larger doses to achieve the desired effects; this leads to dependency and, shortly after, withdrawal symptoms when they try to reduce or stop usage.
Why are Benzos Difficult Drugs to Quit?
Benzos are challenging to quit due to physiological and psychological dependence. Upon prolonged use, the brain adjusts to the presence of these medications; this alters neurotransmitter levels, particularly GABA, which leads to decreased natural production. As a result of this, when individuals attempt to quit, they experience withdrawal symptoms. Some of these symptoms may include anxiety, insomnia, irritability, and seizures.
Additionally, users may develop a psychological reliance on these drugs as a coping mechanism for stress or anxiety. This makes the prospect of quitting not only physically daunting but also emotionally distressing. This dual nature of dependency emphasizes the importance of a careful and medically supervised tapering process for those looking to discontinue use.
The Impact of Physical Drug Dependence on Withdrawal Timelines

Physical drug dependence can significantly influence the withdrawal timeline; the body adapts to the presence of the substance over time. When a person who is physically dependent on a drug stops using it, the body undergoes a series of physiological changes. This process can lead to a range of withdrawal symptoms, which may vary in intensity and duration depending on several factors. Some of these include the type of drug, the length of use, dosage, and individual health conditions.
Generally, withdrawal symptoms can begin within hours to days after the last use and may peak in intensity during the first week; they’ll gradually subside over a few weeks. However, some individuals may experience prolonged withdrawal symptoms, referred to as post-acute withdrawal syndrome (PAWS). PAWS can last for months and impact emotional and psychological stability.
Relapsing on Drugs That are Hard to Quit
Relapsing on drugs that are hard to quit presents a complex challenge, often involving a multitude of psychological and physiological factors. Many individuals battling addiction may find themselves drawn back to substances, even though they’re trying to remain sober. Emotional triggers, environmental cues, and stress can intensify the circumstances, leading to a cycle of relapse and recovery. Understanding the nature of addiction is crucial. Support systems, therapy, and coping strategies can go a long way in helping those in recovery. Recognizing that relapse is often a part of the recovery journey can also help reduce feelings of shame and guilt. This helps encourage individuals to seek the help they need instead of fearing it.
Getting Help for Addiction to Drugs that are Hard to Quit
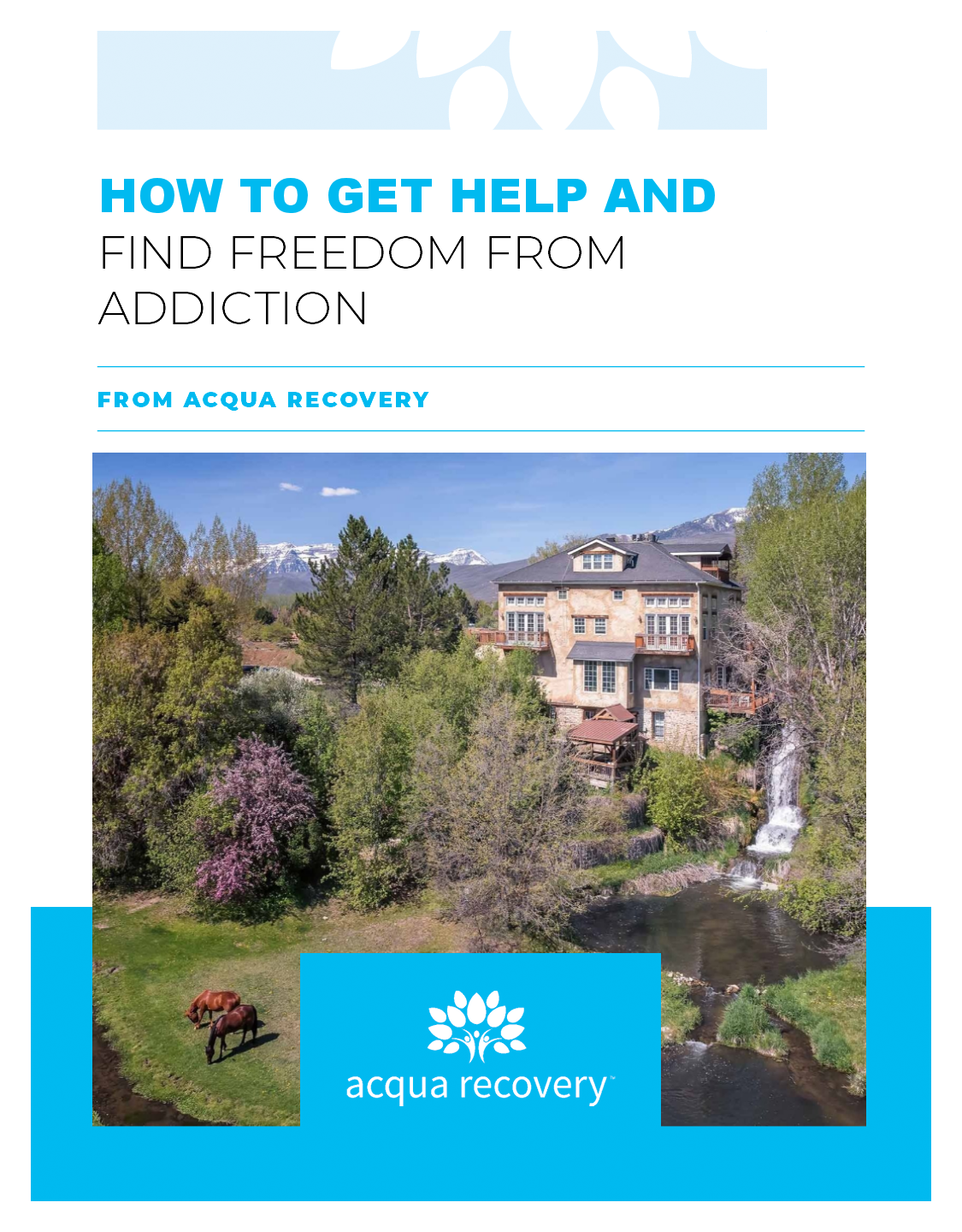
Acqua Recovery offers a supportive and comprehensive approach for individuals struggling with addiction to drugs that are notoriously difficult to quit. With a focus on personalized care, our experienced team provides tailored treatment plans that address the unique needs of each client. We believe in integrating evidence-based therapies along with holistic methods to foster healing and recovery. Our welcoming environment encourages open communication and peer support, empowering individuals to confront their challenges effectively. Acqua Recovery is here to guide you through every step of the journey towards lasting recovery.
Acqua Recovery Can Help You Stop Drugs that are Hard to Quit

Regardless of whatever substance an individual is trying to quit abusing, the journey is tumultuous. This is why we offer individualized care at Acqua Recovery, to give people the best shot at recovering effectively. If you or a loved one would like to find out more, you can contact us here.